Written by Michael Beisty
Disclaimer: The author is not a qualified medical practitioner or accredited coach. The information provided is not intended as medical advice or to replace advice given by trained medical or allied health professionals or qualified coaches. Content herein does not constitute specific advice to the reader’s circumstance. It is only opinion based on the author’s perspective that others may learn from.
Anyone of any age who engages in running, and related exercise, should be in tune with their body and seek medical advice before embarking on an exercise program (including changes to said program) that may unduly extend them. This is critical should the aspiring athlete have underlying medical conditions and/or ongoing health issues requiring medication.
‘The question has never been whether exercise is good for you, but whether extreme exercise is bad for you.’ (Ben Levine 2019)1
‘As athletes age, they’re naturally more prone to developing cardiovascular disease, regardless of how strong their heart may be. Fitness and an active lifestyle can help to protect against this, but not entirely.’ (MedStar Health 2021)2
‘Long-term exercise training induces cardiac remodelling, and limited evidence suggests that this may be maladaptive in some very active athletes.’ (Franklin et al 2021)3
‘While none of us can know for sure that running will add years to our life, there’s no doubt it will add life to our years.’ (Amby Burfoot 2018)4
1. Introduction
Though I have referenced issues relating to the heart in some previous articles for Runner’s Tribe, I have not discussed this topic in any depth. This article is dedicated to a closer examination of contemporary research into the heart health of mature endurance athletes, building upon Parts One and Two of the Fundamentally Speaking series. All of the available literature indicates that the risk of serious heart events for mature endurance competitors is very small, physical activity being highly beneficial to the human body. However, the risks are real for those with particular susceptibilities.
During the past 15 years I have become curious about the workings of the heart and cardiovascular system. More recently I’ve been investigating related issues to inform my attempt to devise an age-appropriate training program for distance runners over 60. While we are told that endurance exercise is a healthy past-time, as we age arguments are put that we may need to be circumspect about the extent to which we engage in such activity, as it relates to the volume and intensity of training.
I regularly hear about cardiac conditions that have arisen for runners in their later years that may have resulted from excessive endurance activity. Anecdotally, some triathletes also appear to have a high susceptibility to heart conditions. From my reading of the current literature, the main dangers appear to be increases in coronary artery calcification (CAC) and the development of atrial fibrillation (AF).
Naively, I was hoping to provide some clear answers to the questions of volume and intensity. However, by researching this article I found that heart physiology is a hugely complex field, affected by a multitude of biological interplays, genetic disposition, and a range of variables that include an individuals’ tolerance for, and response to, physical activity. As La Gerche has indicated the relationship between heart health and exercise is not a binary equation, it is incredibly nuanced.
In terms of disclosure, the bulk of this article is a patchwork of direct excerpts and quotes from research studies and YouTube podcasts (abridged verbatim) joined together in a summary format. Hopefully, this provides a coherent narrative for the article. As much as possible, I have used simple language, applied a layperson’s interpretation, and guarded against providing information out of context. However, the topic content is a dense read. Inevitably, given the complexity of related issues, gaps in my knowledge may become evident to some readers. I advise the mature reader to view this article as a jump off point to explore the source material for detailed and expert information straight from the horses’ mouth.
2. Research Studies
In preparing this article I have considered a number of research studies/reviews that may increase our understanding of related issues:
Franklin et al (2020)5 examined the benefits and risks of physical activity/exertion by men and women in varied environments and during competitive events, and what it means for appropriate preparticipation screening.
Parry Williams et al (2021)6 conducted an extensive review of studies of lifelong male athletes over the age of 40 and impacts on heart health, compared to relatively healthy sedentary controls.
Moorman et al (2021)7 conducted a clinical review of research/studies to inform an appropriate program and rationale for the cardiovascular risk assessment of older athletes, greater than 35 years of age.
Aengevaeren et al (2023)8 examined the longitudinal relationship between exercise training characteristics and coronary atherosclerosis. Participants numbered 289 men, aged 50 to 60 years old [median age 54]. This study has been referenced extensively in an edition of The Older Athlete You Tube series titled How hard to train? A cardiologist on heart health for older athletes discussed in another section of this article.9
I have also sourced You Tube interviews with Dr Ben Levine10, Dr Peter Attia11 and Prof Andre La Gerche.12 Levine, a cardiologist and cardiovascular physiologist, is a highly respected researcher in the field of endurance exercise and the heart. His work is extensive and has been conducted over many years. Attia is a physician and researcher well known for his work in ‘longevity’ and the development of the 4 pillars of exercise model (stability, strength, aerobic efficiency and anaerobic performance). La Gerche is an eminent sports cardiologist at St Vincents Institute of Medical Research in Melbourne and an active mature age endurance athlete.
3. Some Basic Heart Facts
The cardiovascular system (blood circulatory system) plays a significant role within the human body. This system is made up of the heart and blood vessels running through the entire body. In very simple terms the heart is a muscle that works as a pump. It receives blood via coronary arteries and contracts to move blood (containing oxygen and nutrients) to all tissues of the body. Veins then carry the deoxygenated blood back to the heart, which then pumps it through the lungs for a fresh supply of oxygen.13
There are four chambers to the heart. The left and right atria are the upper chambers, responsible for priming the blood, and the left and right ventricles are the lower chambers, responsible for pumping the blood.
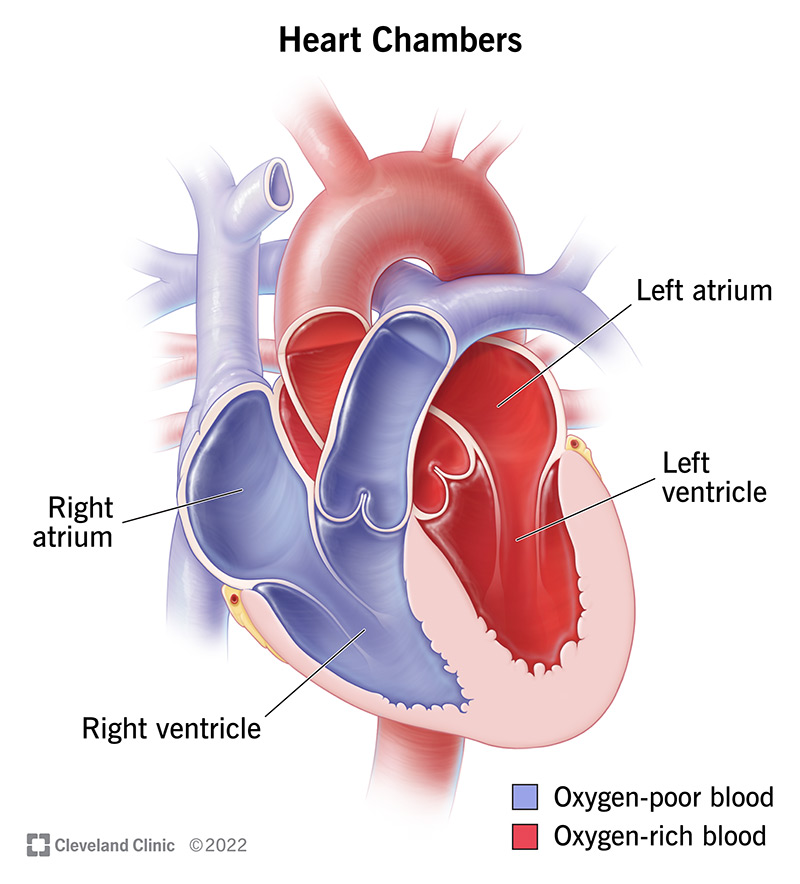
What is the cardiac conduction system? This is a special electrical system within the heart that controls the rate and rhythm of the heartbeat. With each heartbeat, an electrical signal travels from the top of the heart to the bottom, causing the heart to contract and pump blood.14
Levine has stated ‘We think of endurance as primarily the repetitive contraction of large muscle groups, and as you do that and increase the metabolic demand in skeletal muscle, it is the skeletal muscle that drives the cardiovascular response to exercise. The heart has to dilate to get bigger to pump the blood back. It is the ability to dilate and accommodate a large amount of blood flow, the ability to pump a lot of blood (stroke volume) that absolutely distinguishes the elite endurance athlete from the sedentary individual.’15
With increasing age there is a progressive decrease in contractility, efficiency and fatigue resistance of the heart and skeletal muscles. There is also a progressive fall in the capacity to deliver oxygen to the myocardium (thick middle layer of the heart) caused by changes in, or disease of, the coronary blood vessels.16 Levine advises that a progressive stiffening of the heart occurs up until the age of 55. Thereafter, it doesn’t get a lot stiffer, instead it starts to shrink.17
It is known that ageing affects the plasticity of the heart and the heart atrophies through inactivity, so continuing to exercise in later years mitigates the stiffening that occurs through ageing and guards against increased deterioration through inactivity.18
What is atherosclerosis? The buildup of fats, cholesterol and other substances in and on artery walls. Commonly known as plaque, this can cause arteries to narrow, blocking blood flow. If the plaque bursts this can lead to blood clots.19
Attia has commented that the four main things that predispose you to atherosclerosis are a level of dysfunction relating to metabolism, lipoproteins, inflammation, and the endothelium, or a combination thereof.
What is coronary artery calcium (CAC)? ‘It is a highly specific marker of atherosclerosis that has prognostic value in predicting cardiovascular risk.’ Described as ‘calcium deposits in the coronary arteries that occur during atherosclerotic plaque formation.’20 Robust evidence supports a significant association between elevated CAC and the risk of future atherosclerotic cardiovascular disease (ASCVD), independent of traditional risk factors or symptoms.21
What is a coronary artery calcium score? Measures the amount of plaque built up in the walls of the arteries of the heart, the cholesterol in arteries that becomes calcified.22 CAC is quantified as the Agatston score; a score of >400 is severe, 101 to 400 is moderate, 11 to 100 is mild, and 1 to 10 is minimal.23 While it is not possible to reverse or reduce this score, it is possible to reduce the risk of a heart attack through diet, exercise and other lifestyle changes.24
While agreeing that a CAC score may be a predictor of the future risk of a cardiac event, Attia states that it is not a biomarker, it is ‘a backwards looking piece of evidence that you have disease and that damage has already occurred to the artery.’

Source: Fun Runner Vol 4 No 3 Photographer not credited.
.
What is a myocardial infarction (MI)? Also known as a heart attack, this is the injury to, or death of, the heart muscle. Heart attacks are typically caused by blockages in the coronary arteries. Referred to as coronary artery disease (CAD), it is known in Australia as ischaemic heart disease. The most common underlying cause of heart attacks is atherosclerosis.25
Common warning signs and symptoms include chest pain/discomfort (which can radiate to other parts of the body such as the arms, back, neck, jaw, or stomach), unusual shortness of breath, nausea, light-headedness, looking pale, and perspiring. Though chest pain and discomfort are commonly experienced by men and women, it is well documented that women often experience, more than men, the more subtle ‘radiated’ symptoms, which they can tend to ignore.
What is myocardial fibrosis? The scarring of your heart muscle. Heart attacks are the leading cause. However, any condition that damages your heart can lead to myocardial fibrosis.26
What is atrial fibrillation? ‘AF is characterised by chaotic electrical activity that replaces normal sinus rhythm (pattern of your heart beat) and eliminates the contribution of atrial contraction to left ventricular filling.’27 AF is the most common arrhythmia in the general population, and the risk of AF depends on subject characteristics, health status, lifestyle factors, obstructive sleep apnea and cardiac characteristics.
What is a cardiac arrest or sudden cardiac arrest? This is when the heart stops beating; it stops working as an effective pump. Cardiac arrest is caused by heartbeat irregularities, due to electrical malfunctions in the heart.28 Common warning signs and symptoms are a sudden loss of consciousness, absence of pulse or heartbeat, stopping of breathing, and pale or blue-tinged skin.
What is athlete’s heart? Exercised induced cardiac remodelling, known as athlete’s heart, is ‘a physiological response where the heart becomes larger and more efficient than average as a natural response to exercise.’29 This is normal. The increased heart size means that more blood can be pumped with each stroke, causing a reduction in resting pulse rate. However, in some instances an abnormal enlargement of the heart muscle can develop. For instance, pathological conditions such as hypertrophic cardiomyopathy are characterised by an abnormal thickening of the heart and stem from a genetic disorder. The abnormally enlarged heart doesn’t function as efficiently as a healthy heart.
Sudden cardiac death (SCD) can occur in younger athletes under 35-40 years of age who may have ‘genetic or congenital cardiovascular conditions, including coronary artery anomalies, hypertrophic cardiomyopathy, and inherited arrhythmia syndromes.’30
As a generalisation, in younger individuals, concerns tend to centre on congenital heart conditions. For mature individuals it can revolve moreso around CAD that develops gradually over many years. This appears to be a proven trend discussed in all the available literature.
4. Research Discussion
Eminent practitioners in this field note the lack of comprehensive research into the effect of endurance exercise on the mature endurance athlete’s heart and cardiac function, even less so for the elite among them, and those past middle age. The research that has been done is only the beginning of more detailed studies required to achieve conclusive results. Much of the existing research is biased to a man’s experience, making it difficult to draw reliable conclusions about women. In other words, we are at the preliminary stage of understanding the cardiac implications of higher volumes and intensity of endurance training on all mature competitive athletes. However, there has been increased activity in this field by contemporary sports scientists and researchers that has identified potential themes and started to frame a narrative.
I accept with confidence Franklin et al’s statement31 that based on substantial research ‘regular physical activity and higher cardio respiratory fitness both delay the development of atherosclerotic cardiovascular disease (CVD) and reduce the incidence of coronary heart disease (CHD) events.’ They continue that a large number of studies have proven that increasing volumes of physical activity result in significant risk reductions for cardiovascular mortality and all-cause mortality. And when combined with lifestyle changes, moderate to vigorous physical activity can increase life expectancy for men and women.32
Though it is well proven that appropriate exercise is of benefit to the heart, in 2003 Noakes33 stated ‘some recent studies suggest that there may be some detrimental consequences of acute prolonged exercise, such as ultramarathon running or completing the Ironman, or of very high levels of activity sustained for many decades.’ Twenty years on, based on current research studies, and his own lived experience, a similar inference has been drawn by Peter Reaburn, Retired Professor of Exercise and Sports Science.
An emerging body of research, though not conclusive, indicates that mature endurance athletes with a lifetime of high intensity training and racing may be more susceptible to a range of heart conditions. This research shows that ‘chronic’ long term endurance training at ‘vigorous’ (vs moderate) intensity may increase the instance of some CVD risk factors and conditions. Reaburn has voiced specific concerns about engagement in frequent high intensity sessions and regular at threshold or above continuous training for the lifetime competitive endurance athlete.34 To reduce the long-term risk of AF or other cardiac complications, Reaburn’s advice for ‘older’ mature athletes is to cease long threshold training. Instead, he opts for regular low-moderate training, and threshold or high intensity interval training (HIIT) only once per week.35
Of academic interest, Noakes makes plain his disagreement with the traditional physiological model of athletic exercise, that he describes as the Cardiovascular/Anaerobic model.36 This model contends that muscle fatigue, particularly during high intensity exercise of short duration, occurs when the exercising muscles requirement for oxygen is greater than the heart’s ability to meet that demand, and the muscles are forced to contract anaerobically. He indicates that if the body did in fact behave in this way, given the heart is also a muscle, it would lead to heart fatigue and ultimately heart damage of a healthy athlete through anaerobiosis. Following such a model to its natural conclusion would mean a healthy athlete ceases exercising because they experience chest pain resulting from inadequate oxygen supply to the heart, which clearly does not occur. Noakes points to this models’ inherent contradiction: how can the blood supply to skeletal muscles be inadequate while supply to heart remains adequate?37
Noakes contends that it is the hearts’ blood pumping capacity that may limit maximal aerobic exercise performance and the maximal blood flow to the heart, preventing any potential damage to the heart itself.38 And that a central governor, likely the brain, puts the brakes on continued recruitment of additional muscle fibres that would otherwise be used to increase the work output and oxygen consumption and thereby precipitate myocardial ischemia and anaerobiosis. In other words, upon receiving signals from the heart, the brain in anticipation of the likely damage to the heart of continued high intensity exercise, terminates the exercise to prevent any harm.
5. Clarkson’s Observations
Many readers will be aware of the Older Athlete You Tube series, what I consider to be a natural response to the increased numbers of mature individuals competing in endurance events and wanting to better understand the effect of training/exercise on a mature person’s physiology. In one edition titled How hard to train? A cardiologist on heart health for older athletes, Scottish cardiologist and climber, Dr Peter Clarkson, makes a number of observations when referencing the results of the Aengevaeren et al (2023) research study. The point is made that Clarkson’s comments do not constitute specific medical advice, and that further outcomes of this ongoing longitudinal study are yet to be known.
This research involved Measuring Athlete’s Risk of Cardiovascular Events, and is known as the MARC study. MARC-1 participants totalled 318 men. MARC-2 participants (289) were followed up six years later. The major finding was that exercise intensity, but not volume, is associated with the progression of coronary atherosclerosis. Of note, very vigorous intensity exercise (>9 MET hours per week) was associated with greater CAC and calcified plaque progression, whereas vigorous intensity exercise (6 to 9 MET hours per week) was associated with less CAC progression.
[As I stated in the introduction to the Fundamentally Speaking series, many studies tend to focus on the mature endurance athlete as a homogenous group across all sports disciplines, coalescing the experience of individuals across multiple disciplines such as running, cycling, swimming and skiing etc. To enable fair comparisons, volume and intensity is sometimes measured in research studies by what is described as a metabolic equivalent of task (MET). One MET is approximately 3.5 millilitres of oxygen consumed per kilogram of bodyweight per minute, expressed as 3.5mL oxygen uptake/kg/min.]5.1 Summary points from the Clarkson interview are:
Older endurance athletes appear more prone to calcification (hardening of the arteries) and AF.
In terms of calcification:
- Calcification is more common in men than women.
- Calcification is more prevalent in those doing a high percentage of very vigorous exercise.
- Calcification doesn’t appear to be affected by the overall duration of exercise.
- It is clear that an older endurance athlete should not do solely high intensity sessions.
- Though high intensity activity is good for the body, VO2 max and performance, to lower the risk of calcification mature athletes also need to engage in a significant amount of low intensity exercise.
- Endurance athletes shouldn’t stop doing high intensity workouts because of this small risk of calcification. However, Clarkson suggested using the proportion of 80% low intensity (conversational) and 20% high intensity. An 80:20 rule of thumb. A 50:50 ratio presents a much higher risk of calcification.
- We do not have a biomarker that measures calcification, the only accurate means of assessing calcification being CT scans and X rays. These are not recommended unless absolutely necessary because of the level of radiation to the chest.
- This may mean that endurance athletes are more prone to angina than necessarily having a heart attack. Noting that hard calcified arteries provide a lesser risk of heart attack when compared to the existence of fatty plaque within arteries, the latter presenting a more imminent risk of blockages.
- A red flag for heart issues is suffering from a central chest pain that is difficult to localise.
In terms of AF:
- Symptoms include a combination of erratic pulse rate, palpitations, feeling more breathless (feel capped on exercise), and typically starts with little bursts (paroxysms that last a few minutes then reverts itself to normal) that become longer and more frequent over time until eventually it results in persistent/permanent AF. [paroxysmal supraventricular tachycardia (PSVT) is episodes of rapid heart rate that start in a part of the heart above the ventricles]
- Those who do a lot of endurance activity are more prone to AF (chaotic rhythm of atria) and atrial flutter (caught up in an electric circuit, 5 times per second, ongoing cycle).
- AF presents a small but definite risk of stroke (coagulated blood that can travel to brain).
- Those at greatest risk of AF are those who do very little and those who do a lot of exercise.
- According to some studies, every 10 years of heavy exercise your risk of AF and flutter increases by 16% and 40%, respectively.
6. Other Studies
As you may expect Clarkson’s comments reflect much of the Parry-Williams et al and Franklin et al research. However, a few things were particularly noteworthy within these studies, and others:
6.1 The Parry-Williams study states that the first order benefit of regular physical exercise is its positive impact on atherosclerotic risk factors such as blood pressure, lipid profile, body mass index and insulin resistance. The improvements in cardiovascular risk profile being secondary, though significant, outcomes.
They also state that while regular physical exercise is clearly beneficial to the human body, reducing the overall risk of atherosclerosis, there is no evidence suggesting that any one exercise type has a preferential benefit on endothelial function (substances that control the opening and closing of arteries) over another. They go on to say that optimal endothelial function is achieved through regular moderate-intensity physical exercise.
Commenting on the experience of lifelong endurance athletes, whose extent of exercise is typically 10 to 20 folds greater than the minimum recommendations for exercise of the average person, there appears to be a threshold beyond which the benefits of exercise are lost. [Many readers would be aware of minimum guidelines recommending at least 150 minutes of moderate exercise or 75 minutes of vigorous exercise per week].
Further comments include:
‘A small proportion of ostensibly healthy master athletes reveal atrial fibrillation, coronary artery calcification, and myocardial fibrosis, which has increased speculation about the potentially deleterious impact of chronic endurance exercise on cardiovascular health’; and
‘Middle-aged endurance athletes are at a five-fold increased risk of atrial fibrillation compared with sedentary counterparts……..Extrinsic contributing factors include male sex, tall stature, and the volume and intensity of exercise.’
This study provides some information about the differences between men and women. Notably men appear to have a higher relative risk of SCD and MI from exercise. ‘Risks appear to be highest in men unaccustomed to exercise, with substantially lower risks in regular exercisers and women.’ The study notes that when expressed as an absolute risk, such acute events are very rare, and goes on to say that ‘the most common cause of exercise related SCD in middle aged and older adults is atherosclerotic CAD.’
Referencing the incidence of calcification in masters’ women, there is a suggestion that female athletes may benefit from the protective effect of oestrogens pre-menopause; however, it’s noted that the related studies are very small and caution is warranted; realistically, the effect of menopause on the prevalence of CAC is unknown.
6.2 Franklin et al note that most studies, but not all, have reported a decrease in cardiovascular events with increasing regular physical exercise. Despite these long-term benefits, the risk of SCD and MI is increased during and shortly after bouts of vigorous physical exertion.
They also state that collectively the data they examined ‘suggest that athletes with CAC are at higher risk for mortality and acute cardiac events than athletes without CAC; however, the risk for adverse cardiovascular outcomes is lower in physically active people than their inactive counterparts with the same CAC score.’
6.3 Moorman et al, concur that CAD is the leading cause of SCD in older athletes. They suggest the use of CAC scores to reclassify risk as part of a suite of options to inform treatment decisions. And that stress testing be used for symptomatic athletes, typically those who are considered high risk for atherosclerotic cardio vascular disease and/or those engaged in strenuous exercise. Though, the Cardiac Society of Australia and New Zealand (CSANZ) does not recommend CAC scoring for high and low risk patients, where there is little likelihood of a change in risk profile as a result of such testing, preferring a focus on intermediate risk patients.39 Of note, studies of endurance athletes demonstrate a higher prevalence of CAC compared with matched nonathletes with similar risk profiles and the coronary plaque composition in athletes is more benign, comprised of more calcified and stable plaque.
Distilling the Moorman et al study, it may not be unreasonable for older endurance athletes to have an initial CAC test to benchmark their level of calcification. Annual monitoring of heart health can be achieved through appropriate blood tests (blood lipids) and measuring blood pressure. Of course, stress echocardiogram and electrocardiogram (ECG) tests may also provide peace of mind. However, all of these issues have to be considered through consultation with appropriate medical practitioners.
7. Putting CAC and AF in Context
In terms of relative risk, based on research studies and their own knowledge La Gerche, Levine and Attia appear to express greater concern about AF than CAC.
7.1 Coronary Artery Calcification
7.1.1 Attia makes the following points concerning CAC scoring and calcification:
A CAC score derives from a CT scan done without any contrast. It does not show how much narrowing has occurred in the arterial lumen. The amount of calcification is scored and ranked against a percentile. Calcium scores are helpful [author’s comment: but not categorical] in estimating the risk or probability of a major adverse coronary event (MACE) such as a heart attack, stroke or cardiac death. For instance, a score of zero, or a negative score, doesn’t mean you have no risk whatsoever. Rather, it means actuarily at the population level there is a lower risk of a MACE occurring.
If the scan shows calcification this indicates the individual has already had an advanced lesion(s) and that lesion(s) had to be repaired (reflected by hardening). Attia states that ‘calcification is an incredibly late stage repair, so when you have calcification in a coronary artery you’ve had real damage and it has been repaired, and that becomes a marker of risk..’
A person with a zero score could have plenty of ‘soft plaque’ and/or other arterial damage, that has not shown up at the stage of calcification through the CT scan. Soft plaque is also a significant marker of risk and a cause of MI. There is some thought that a higher density of calcified plaque, reflected in CAC scores, results in a greater stabilisation of your condition, when compared to soft plaque, and therefore you could argue it means a lesser risk of a coronary event. [Author’s comment: You can think of it in these terms: the score will increase as plaque stabilises and hardens, so with a much less likelihood of a rupture, the risk of a coronary event actually reduces].
Attia stresses that the score number is not as important as the percentile: the rate compared to your peers by age and gender. For example, a person aged 35-40 years old with a score of 6 is at a much higher risk of a MACE, now and into the future, than a person aged 80 with the same score. The latter would be considered quite low, but the former sits at the 75th to 90th percentile for their age.
7.1.2 Levine is an expert in the field of calcification and expresses similar views to Attia about CAC scores. Levine has a collaborative relationship with the Cooper Institute of Dallas Texas, a research and education organisation in the field of health. Its origins stem from the work of the Father of Aerobics, Dr. Kenneth H. Cooper. Levine advises the following:
Atherosclerosis develops and heals by a process of calcification. He further states that calcified blood vessels don’t rupture and the calcium score is purely an index of the volume of atherosclerotic plaque (the more calcium you have the more atherosclerosis you have).
He cites cross-sectional studies of marathon runners suggesting that athletes might have more calcification than not. However, when examined more closely in a UK study by using coronary CT angiograms it was found that while athletes did have more calcification, they did not have more non-calcified plaque. So, you could argue that despite the score they could be considered at less risk of a coronary heart event.
Further, Levine cites outcomes of a longitudinal study done in collaboration with the Cooper Institute, involving the experience of male endurance athletes.40 In this study they quantified the physical activity of a large sample of athletes over many years who were followed for mortality. Coronary artery calcium was measured as part of the study. Athletes were grouped based on levels of physical activity:
Low: less than 1 hour pw
Moderate: 1-8 hours pw
High: more than 8 hours pw
Further sub-categorisation was based on a score of less than and greater than 100, when risk of coronary events starts to increase.
Some specifics of the study are:
Period of measurement: 1998 to 2013 (15 years)
Number of Participants: 21758 men
Age: 40 to 80 years old, generally middle aged and healthy, without cardiovascular disease
Exercise Modality: Predominantly runners, and some cyclists, swimmers and rowers plus a sub-group who trained in all three of the latter
High intensity, high volume was defined as at least 5 to 6 hours per week at 10 minutes per mile (6:12 km pace)
The study found absolutely no difference in the volume of coronary calcium between these groups. He concludes that there is no evidence that exercise training increases the coronary artery calcium score, though it did increase the risk of having a high calcium score, a subtle difference, also described by Attia. The high physical activity group who scored less than 100, had a 50% reduction in their rate of death or having a cardiovascular mortality while those who scored over 100, had a 25 % lower risk.
Specifically, the study showed that
- there is a slightly greater risk (11%) of having a high calcification score, for those who do a lot of exercise;
- the volume of training did not increase the risk of having more calcium but did increase the risk of having a higher calcium score; and
- being highly physically active, if you have a little bit of calcium, may be protective.
Overall, Levine interprets these results as meaning ‘higher amounts of physical activity does not cause higher levels of coronary calcium, and does not increase mortality, if anything it reduces mortality.’ Or expressed another way, the topline outcome was that high volumes of exercise are safe and the benefits of exercise far outweigh the minor risk of having a little more coronary calcium.
Levine states that extreme duration exercise like ironmen events and ultra-marathons are done at low intensity. He refers to a proven increase in vasodilation function (widening of the blood vessels) by ultramarathoners. He cites another study of 66 men who exercised more than 10000 MET minutes per week (30 hours per week). He considers that given there were no cardiovascular deaths amongst this group, it is premature to worry about extreme exercise at least for coronary calcium.
Levine cautions that running with ischemia (occluded arteries) is not good for the heart and there is some data suggesting that this induces scarring. It is unwise to ignore symptoms such as tightness and pressure while exercising, particularly if gets worse when running and eases when you stop. Medical advice should be sought.
7.1.3 La Gerche cites recent research showing that lifelong athletes, more than recent athletes, and more than controls, experienced increased calcium, higher rates of coronary disease, and higher rates of proximal disease. Every picture of coronary health looked worse in the athletes yet the epidemiological evidence is that there are fewer heart attacks, clinically. La Gerche attributes this to a higher order statin-like effect of sport and exercise (use of statins increases the coronary calcium score, and there is this concept that it hardens the plaque and it acts as an anti-inflammatory, and as part of that process you get some calcium deposition). He notes that Levine attributes a relative risk reduction of a heart attack at about 60% for a fit endurance athlete, whereas statins typically provide a 20-25% reduction in risk.
The reasons for increased calcium associated with a lot of exercise aren’t clear, though it could be a result of the sheer stress on the heart, or micro damage. [Author’s comment: Attia and Levine have made similar statements]. Although 20-30% of the average population go through life with whistle clean arteries, generally, arteries become more calcified with age. While fitness can provide a relative insurance policy against the risk of heart attack, reducing the odds against it, it can’t guarantee you will never have a heart attack, and heart attacks are common. However, the fitter you are, for any degree of calcium you have (measured by a CAC score,) your risk of heart attack is lower.
When it comes to coronary artery disease, and the buildup of plaque, it does seem that women are relatively protected before menopause and then the risk accelerates a bit but they do remain protected matched age to age with men throughout life and the only time you see an excess for women is in the later decades, mainly because the men are gone (shorter lifespan). There is something that seems to make a woman’s heart more stable. It’s not well understood. It doesn’t seem to be greatly affected by menopause or a hormonal oestrogen/testosterone issue.
7.2 Atrial Fibrillation
La Gerche, Levine and Attia indicate that there is a strong evidence base, and little doubt, that doing a lot of endurance exercise increases the risk of AF: up to a five fold increased risk above the population of AF, the non-competitive less so.
In explaining the reason why AF can occur in elite endurance athletes who are engaged in extreme exercise, Attia describes the heart as a muscle whose electrical system exists within the wall and the more often it is stretched, and held for long periods of time in a stretched position, the more you are damaging the electrical architecture of it.
7.2.1 Levine describes AF in the following terms:
Essentially the atria are the collecting chambers and they prime the ventricles. They sit at the top of the heart and the heart fills into the atria, like a reservoir, then they prime the pump just before the heart contracts. The body’s pace maker sits in the upper righthand corner of the right atrium. That’s what initiates the regular heartbeat. Many different cells within the atria can take over and have their own electrical activity. When this happens, electrical activity can get very chaotic and the heart can beat irregularly and fast. This can reduce performance, make you feel bad, and increase the risk of stroke.
Levine cites a Norwegian study of people over a 30 years period that examines their risk of AF and the relationship with exercise. The major finding was those who engaged in a low level of exercise, or no activity at all, were at high risk of AF, those engaged in extreme exercise increased their risk by up to twofold, with elite athletes’ risk being fivefold. It seems that the lowest level of risk was experienced by those who exercised at moderate to high levels.
Why is this so? Levine explains that during exercise the valves between the atria and the ventricles close up to allow the blood to pump out of the aorta and pulmonary artery. As you increase the heart rate you increase the amount of time the body spends with the valves closed and at the same time you are pouring blood into the atria, so the atria distend and stretches. Levine cites a study that links an increased risk of AF to the thinner walls of the atria, that are more likely to dilate with exercise than the ventricles.
There is a view that because women don’t get the same hypertrophic stimulus (causing enlargement in muscular cells) that men do from training, they may be protected from this dilation to some degree, when compared to men.
In addition, Levine cites the Australian research of La Gerche (refer below). He explains that the smaller right ventricle is most susceptible to fatigue and injury, and that for a small number of people who exercise excessively this can cause the development of arrythmias, notably ‘exercise induced right ventricular cardiomyopathy.’ He also references right ventricular cardiomyopathy as a genetic disease that can present a higher risk of a cardiac event, that can result in a rapid progression towards life threatening arrythmias. Having an underlying genetic abnormality of the right ventricle is clearly dangerous.
7.2.2 La Gerche describes AF and related issues as follows:
The atria, or priming chambers, are thinner walled compliant balloon like things that can fill with blood and help push that last bit of blood into the ventricles to prime them and make them even more efficient. AF is when the atria have an irregular rhythm, are out of coordination and the pulse becomes chaotic. Some people can be very disturbed by the feeling, and others don’t even notice when they go into AF. Importantly it never causes sudden deaths. La Gerche describes it as a ‘nuisance arrhythmia’ not a life-threatening arrhythmia. But he does proffer that it can increase the risk of having a stroke because this chaotic activity is more likely to form clots, and it can affect the heart function over time.
Based on a study of professional rowers (ex-Olympians), and studies of other endurance competitors, La Gerche considers that the risk of AF can be up to 7 times more in endurance athletes.
AF is very common. By age 80, 10 per cent of the general population has AF. For endurance athletes there is difficulty disentangling the cause/risk of AF from the natural ageing process and sport activity/exercise. And the question is often asked should you cutback? Was it caused by exercise or would it have happened anyway? Because exercise has so many benefits, La Gerche’s default is if in doubt keep exercising, until proven otherwise. He acknowledges this may differ from the advice of his colleagues.
La Gerche has investigated the occurrence of arrythmias and heart rhythm issues emanating from the right ventricle. As part of his investigations, he found that for those athletes who are able to compete really hard over long distances for several hours, like an ironman triathlon, the right ventricle is abnormally affected immediately after the race (though it would then recover), whereas the left ventricle was okay. He based this on pre and post event imaging.
He states that in simple terms, the body is built for the average setting and when engaged in extreme exercise the heart is put under significant stress. The left ventricle is better built for exercise because its bigger and thicker and can generate more pressures whereas the right ventricle is about one quarter as thick and normally when not exercising it hardly has to push any pressure (it’s very easy to push blood through the lungs). During exercise, flow increases and the right ventricle has to increase disproportionately from virtually no activity to a lot. In a recent study La Gerche has quantified increases in wall stress as 122% in the right ventricle and 30% in the left ventricle. So, in summary, while the whole heart has to work harder and gets bigger with exercise, the right ventricle gets much bigger relative to the left ventricle.
La Gerche states that humans, in some ways, are not built for exercising at these extreme levels for 8 or 9 hours. Although La Gerche is not saying athletes shouldn’t compete in ironmen events, his view is that you do need to pay respect to recovery after events like this. A small number of competitors may experience right ventricles that suffer minor injury, and of that small number, a very small number will experience heart rhythm issues like ventricular tachycardia.
Ventricular tachycardia is an extremely rare condition, where the heart is beating regularly but very fast. It is an emergency situation that can lead to ventricular fibrillation which is catastrophic often resulting in death. In La Gerche’s experience it is more common in endurance athletes and more commonly comes from the right ventricle. It can result in a defibrillator being implanted, which has occurred in elite triathletes and cyclists.
Although women’s risk of many of the arrhythmias and heart attack is less than men, the same patterns exist in women as men. In general AF for women tends to occur at an older age and it is about four or five times less common, as is sudden death. Despite a lack of studies relating to women, it is quite clear that intense endurance sports are associated with an increased risk of AF for women.
-
Can you do too much exercise?
8.1 Levine is unequivocal in addressing the question of Can you do too much exercise? maintaining that in the vast majority of cases a sustained dose of high intensity regular exercise is good for you.
To explore this issue, Levine worked in collaboration with the Cooper Institute and identified a group of elite masters’ athletes, who were highly competitive, and trained 10 to 15 hours per week. He states that their hearts looked like a healthy 20 years old’s. However, this is not a good fit as a public health measure.
So, another question was posed for further research: how much exercise do you need to do over a lifetime to preserve the function of the heart? In a further collaboration with Cooper Clinic a cohort of people were identified who over a 25 year period reported the same amount of exercise every time they visited Cooper Institute doctors. The study excluded anyone with hypertension. There were a range of exercise modalities, not just running. A limitation of the study was that it was based solely on the frequency of activity and not intensity. Reliable measures of intensity over many years would not be possible to obtain. To measure their cardiac and cardiovascular compliance, the study subjects were divided into four categories:
Sedentary: no regular exercise
Casual Exercisers: 2-3 days pw
Committed Exercisers: 4-5 days pw
Highly Competitive: 6-7 days pw
The major finding was the activity of Casual Exercisers had no impact on heart structure and the activity of the Committed Exercisers had nearly as much impact on heart structure as those of the Highly Competitive (elite). Recognising that we are talking only about protecting the cardiac structure (and not other benefits such as metabolic and autonomic changes that can result from most activity, including lower level), Levine concluded that being a Committed Exerciser was the ‘prescription for life’ to optimise cardiac health. He suggested the following routine as an optimal lifetime exercise schedule to train for health:
1 day pw long duration (at least one hour) and fun;
2-3 days pw moderate to vigorous intensity of 30 minutes duration (talk but can’t sing);
1 day pw more intense activity such as the 4×4 Norwegian ski team workout [author’s note, described in research studies as a HIIT protocol, which is 4 minutes at up to 95% VO2peak with 3 mins break, repeated 4 times]; and
include 1-2 days pw of strength training.
He cautioned that despite the benefits of physical activity a bad diet will not be overcome by exercise. Exercise is one component of a number of other requirements to deliver good cardiovascular health.
8.2 On related issues, La Gerche has the following insights:
The body has a reserve that lessens through life and the heart is the same but if you are an athlete the one thing that is absolutely unchangeable is the more you train the more the cardiac output and the slower the degradation.
We don’t have anything that can accurately predict a heart attack, or measure the potential impact of genetics, though it is accepted that genetics can play a role.
An exercise paradox exists, whereby if you are a runner, overall, you will have less risk of heart attack but if you are going to have a heart attack it is more likely to occur while running. You exercise regularly so that every bout of exercise is less of a relative risk. But exercise is a risk activity that you then do regularly to make yourself lower risk. This milieu of what goes on in exercise may go some way to explaining the scarring in arteries, heart muscle and atrium that can cause a problem for some people. Ultimately it is a transient greater risk. All of this doesn’t mean the running or endurance activity kills a person. In fact, but for the running, death may have occurred earlier. Or it may not have. There is no real way of knowing.
-
What does it all mean?
Various descriptors such as ‘excessive’ ‘extreme’ and ‘chronic’, and ‘very vigorous’ and ‘high intensity’ are used in research studies about endurance athletes as it relates to the volume, duration and intensity of exercise. Based on my limited understanding of these research studies it appears to me there are no absolute definitions of what they constitute (though >9 MET hours per week is defined in some studies as ‘very vigorous’ and the 4×4 is often associated with high intensity interval training, and a percentage of VO2max or VO2peak is sometimes used, as is heart rate). It also seems that in some instances the definitions of ‘high intensity’ or ‘vigorous’ and ‘very vigorous’ exercise used in studies are at the lower end of a competitive club runner or elite athlete’s capabilities. So, from my laypersons’ perspective maybe some of the research outcomes are not as easily translatable to the lived experience of these two cohorts of endurance athletes? But I stand to be corerected.
From theexperts, it seems that on balance, with increasing age, AF presents a greater relative risk for mature age athletes than coronary artery calcification. However, a significant calcium buildup (evidenced by CAC scores), should not be ignored as, by extension, it can indicate that you are developing increased levels of ‘soft’ plaque in your arteries, which does elevate your risk of a heart attack. In all instances it is important to understand that CAC and AF conditions require appropriate medical assessment and/or intervention having regard to the whole health condition of an individual, and not be considered in isolation.
Taking a practical perspective, after examining all of the research covered in this article, how do I think this applies to training? I guess up until now the direct relationship between heart health and training wasn’t foremost in my mind. It was a dormant concern, something I didn’t really think about, but knew it was relevant to the question of ageing, and eventually would require closer attention as I got older.
For what it’s worth, my preferred approach is to apply the middle ground to training: enough volume but not too much, low to moderate intensity in longer continuous runs, and very high intensity interval training only sparingly, instead, opting for what I describe as rhythm repetitions. A gradual approach to training progression that stretches but does not exhaust the individual, while delivering healthy outcomes.
Something along the lines of Clarkson’s recommendation of an 80:20 split between low intensity and high intensity running seems on the mark, though how ‘high’ you are willing to go is a matter for the individual to decide. I note that many studies infer that moderate intensity and volume provide the optimal outcomes for improvements in cardiovascular health and reductions in the risk of CHD. Personally, I’ve drawn a line in the sand at anaerobic intensity for faster work and staying primarily within a zone 4 perceived effort for my higher intensity running, whether continuous running or reps. For despite the enduring benefits of regular physical exercise, I am reminded of Moorman et al’s statement that the risk of SCD and MI is increased during and shortly after bouts of vigorous physical exertion. I am also reminded of La Gerche’s view that the relationship between heart health and exercise is not binary.
In addition, I have applied my learnings about the ageing process to the racing arena. Admittedly this has occurred from a greater appreciation of my physical limitations with increased age, rather than any conscious concerns about heart health per se. That being said, I no longer race half marathons, my upper racing distance being 10 kilometres, conducted a maximum of four times per year. I have found longer races (I don’t mean just running through at an amble) exhaust me to a greater extent than when younger and I have no particular inclination to race a marathon, my last one completed in 1988.
-
Conclusion
I wrote this article out of curiosity, not to be alarmist. For, similar to many others, at age 65, it is my intention to continue competing for as long as I can, while navigating the challenges that ageing can present, good heart health being central to wellbeing and competitive desire.
While I have covered some aspects of heart health, it needs to be recognised that the number of mature athletes whose heart is adversely affected by excessive or extreme endurance exercise is very small. Certainly, advocates of physical exercise such as La Gerche, Attia and Levine, are at pains to explain that the risks from excessive or extreme exercise (however you define it), although not insubstantial for some, do not outweigh the overall cardiovascular benefits derived from a lifetime of physical activity. It is important to maintain perspective, a balanced outlook, in weighing up the pros and cons of endurance exercise for a mature athlete and arrive at an understanding of optimal training and racing for the individual to minimise any risk of cardiac complications.
For the vast majority of athletes there is little doubt that regular exercise extends health span and increases lifespan by improving heart health. However, for a mature runner advancing in age it is prudent to understand the associated risks for the individual, however minor. In practical terms, this means understanding any particular susceptibilities, and mitigating risk, by the adoption of an age-appropriate training program, particularly for those who wish to continue competing at a high level. Engaging in regular health checks, at least annually, is a must to ensure you are on track.
While acknowledging that heart health and the effect of physical exercise on the heart is unique to the circumstances of the individual, within limits, as a mid-sixties distance runner, I have adjusted my training and racing programs, to take into account my known level of risk. As I approach 70 years of age, I am more philosophical in my attitude to racing and training, where the pendulum is definitely swinging towards what Reaburn describes as the ‘value of exercise as medicine.’ But not quite to the more modest ‘prescription for life’ regime recommended by Levine for healthy living.
This doesn’t mean that I don’t compete as fiercely as I always have. But it does mean that I am applying commonsense to my training program in putting my health first.
After all, don’t we all want to be in it for the long haul?
Isn’t that the heart of the matter?
References:
1 Athletes can rest easy: Extreme exercise does not raise heart disease risk or mortality, UTSouthwestern Medical Center, media release, 30 January 2019:
https://www.utsouthwestern.edu/newsroom/articles/year-2019/extreme-exercise.html
2 5 Things Athletes Should Know About Their Hearts, Medstar Health, 9 February 2021: https://www.medstarhealth.org/blog/athletes-heart
3 Franklin, et al, Exercise-Related Acute Cardiovascular Events and Potential Deleterious Adaptations Following Long-Term Exercise Training: Placing the Risks into Perspective–An Update. A Scientific Statement from the American Heart Association, Circulation, 31 March 2020: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000749
4 Burfoot, A, Run Forever, 2018
5 Franklin et al, 2020
6 Parry-Williams et al, The heart of the ageing endurance athlete: the role of chronic coronary stress, European Heart Journal, 22 March 2021: https://academic.oup.com/eurheartj/article/42/28/2737/6179516?login=false
7 Moorman et al, Cardiovascular Risk Assessment in the Older Athlete, Sports Health (Sage), Nov/Dec 2021, extract available: https://pmc.ncbi.nlm.nih.gov/articles/PMC8559005/
8 Aengevaeren et al, Exercise Volume Versus Intensity and the Progression of Coronary Atherosclerosis in Middle-Aged and Older Athletes: Findings From the MARC-2 Study Circulation Vol 147 No. 13, 4 January 2023: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.122.061173
9 Interview by Simon Willis with Dr Peter Clarkson, How hard to train? A cardiologist on heart health for older athletes, 19 February 2024: https://www.youtube.com/watch?v=olg90Dq9ay8
10 Interview by Dr Glenn McConell with Dr Benjamin Levine, Can extreme exercise damage the heart?, Inside Exercise, Number 8, 31 July 2022: https://www.youtube.com/watch?v=WlppG5olndQ
11 Attia, P, MD, Coronary calcium score: what it means and how to interpret your results, 22 April 2019: https://m.youtube.com/watch?v=Z7MrZRInjvI
12 Interview by Dr Glenn McConell with Dr Andre La Gerche, The heart and exercise: Should middle-aged men pull on lycra? Inside Exercise, Number 69, October 2023: https://www.youtube.com/watch?v=bvMUAse5mls
13 DeBakey, M, & Gotto, A, The Living Heart, 1977, p6
14 National Heart Lung and Blood Institute, How the Heart Works: How the Heart Beats, 24 March 2022: https://www.nhlbi.nih.gov/health/heart/heart-beats#:~:text=Your%20heart%20has%20a%20special,to%20contract%20and%20pump%20blood.
15 Levine, 2022
16 Noakes, T, The Lore of Running, 2003, p41-42
17 Levine, 2022
18 Levine, 2022
19 Arteriosclerosis/Atherosclerosis, Mayo Clinic, 20 September 2024
20 Chau, A, et al, Coronary artery calcium in primary prevention, Australian Journal of General Practice, Vol 9 Iss 8, August 2020: https://www1.racgp.org.au/ajgp/2020/august/coronary-artery-calcium-in-primary-prevention
21 Moorman et al, 2021
22 South Denver Cardiology, What Is the Normal Range for a Calcium Heart Score?: https://southdenver.com/what-is-the-normal-range-for-a-calcium-heart-score/
23 Moorman et al, 2021
24 South Denver Cardiology
25 Todorovic, M & Barton, M, What’s the difference between a heart attack and cardiac arrest? One’s about plumbing, the other wiring, The Conversation, 9 September 2024: https://apple.news/AzlHbp0cHTVGBAIm2F1zeRQ
26 Yetman, D, Everything You Need to Know About Myocardial Fibrosis, Healthline 17 May 2023: https://www.healthline.com/health/heart-disease/myocardial-fibrosis
27 Franklin et al, 2020
28 Todorovic & Barton, 2024
29 MedStar, 2021
30 MedStar, 2021
31 Franklin et al, 2020
32 Franklin et al, 2020
33 Noakes, 2003, p867
34 Interview with Peter Reaburn, Maximising Health & Performance of the Masters Athlete, Episode 215, The Physical Performance Show, posted by Runners Tribe 1 June 2020: https://www.runnerstribe.com/podcasts/maximising-health-performance-of-the-masters-athlete/
35 Reaburn, 2020
36 Noakes, 2003, p2
37 Noakes, 2003, pp28-33
38 Noakes, 2003, p33
39 Chau et al, 2020
40 DeFina et al, Association of All-Cause and Cardiovascular Mortality With High Levels of Physical Activity and Concurrent Coronary Artery Calcification, 30 January 2019: https://jamanetwork.com/journals/jamacardiology/fullarticle/2722746
Other Sources:
Seladi-Schulman, J, Understanding Sinus Rhythm, Healthline, 11 November 2021:
https://www.healthline.com/health/sinus-rhythm#vs-heart-rate